Community Health Choices
What is Community Health Choices?
- Is Pennsylvania’s mandatory managed care program for dually eligible individuals and individuals with physical disabilities – serving more people in communities, giving them the opportunity to work, spend more time with their families, and experience an overall better quality of life.
- CHC will improve services for hundreds of thousands of Pennsylvanians.
- It is also a combination of Medicare and Medicaid.
What is Health Choices?
- Is Pennsylvania’s mandatory managed care program for current Medical Assistance (Medicaid) participants.
- Participants receive quality medical care and timely access to all appropriate physical and behavioral health services and/or drug alcohol services.
Understanding Community Health
Eligibility
Health Choices
- Children up to, and including 20 years old.
- Adults
- Some women with breast and/or cervical cancer
- Lawfully present immigrants might be eligible
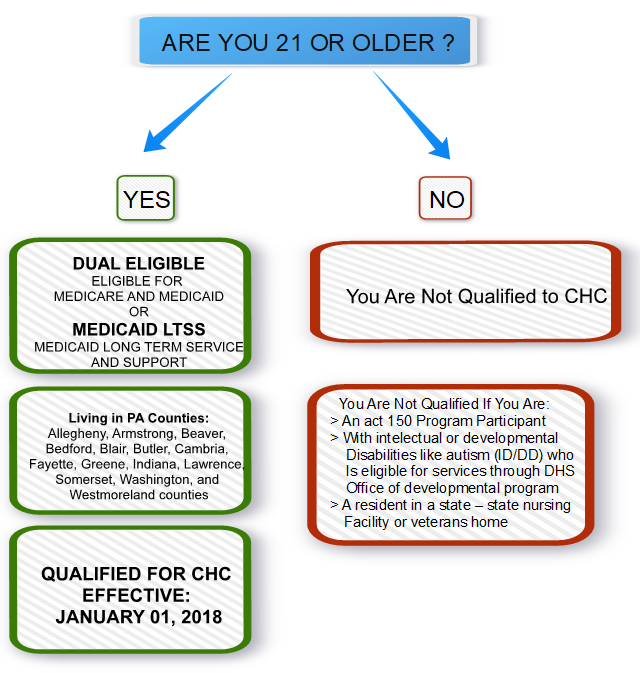
Community Health Choices
- Individuals ages 21 and older who are dually eligible for Medicare and Medicaid
- Individuals ages 21 and older who need the level of care provided by a nursing facility
- Individuals with intellectual or development disabilities who are enrolled in services through the Office of Developmental Programs and residents of a state – operated nursing facility (including state veteran’s homes) are not part of CHC.
What are the similarities between Community Health Choices and Health Choices?
- Both are Medicaid managed care programs
- Both programs utilize manages care organizations (MCOs) to provide coverage for their members.
- The commonwealth pays the MCO’s a capitated monthly rate (like a premium for each member), and the MCOs coordinate the health care needs for their members.
- Zones
- Health choices and CHC use the same five geographic zones.
- Choice
- Members of both programs choose their MCO.
- Physical health benefits
- Health choices and CHC both offer the Adult Benefit Package for physical health services.
- Behavioral health benefits
- Both Health Choices and CHC-MCO are required to coordinate participants behavioral health services with the Behavioral Healthchoices MCO’s.
What are the differences between Health choices and Community Health choices?
Dual-eligible coverage
- CHC provides coverage for participants who are eligible for both Medicare and Medicaid.
- This means that CHC-MCOs will have to coordinate closely with Medicare to ensure that participants have access to comprehensive services.
- Also CHC-MCOs will have the ability to provide Medicare coverage (called D-SNPs) to participants who would like their Medicaid and Medicare services coordinated by the same entity.
- D-SNP’s Dual Eligible Special Need Plans
Long-Term Services and Supports (LTSS)
- Community Health Choices
- Provides LTSS to participants who need the level of care provided in a nursing home.
- Participants who meet this criteria will receive LTSS and physical health services from their CHC-MCO, including nursing facility.
- Health Choices MCOs
- Will cover the first 30 days of nursing facility care. If a participant continues to need that level of care. the participant will apply for CHC.
ADULT BENEFIT PACKAGE FOR ALL CHC PARTICIPANTS
- Home health services
- Hospice services
- ICF/IID and ICF/ORC (requires an institutional level of care)
- In patient hospital services
- Labaratory services
- Maternity (physician, certified nurse, midwives, birth centers)
- Medical supplies
LONG-TERM SERVICES AND SUPPORTS BENEFIT GUIDE
- The following benefits are available to participants who are nursing facility clinically eligible and receive medicaid long-term services and supports through a home and community-based waiver or reside in a nursing facility. These are in addition to physical health benefits in the adult benefit package.
- Home health – physical, occupational, and speech and language therapies
- Specialized medical equipment and supplies