UPMC
UPMC
- University of Pittsburgh Medical Center
- Is committed to providing its members better health, more financial security, and the peace of mind they deserve.
- UPMC Health Plan partners with UPMC and community network providers to produce a combination of knowledge and expertise that provides the highest quality care at the most affordable price
Recipients
- CHC Participants who are eligible and 21 yrs and older.
- Who are dual eligible for Medicaid and Medicare
- Who are qualified for LTSS
How to Check Eligibility
- Log on to https://www.upmchealthplan.com to check eligibility of patient and put the patient’s MA ID.
Prior Authorization
- Prior Authorization is not required for DME Supplies.
Fee Schedule
- 110% of PA Medicaid
Clearing Houses
- WebMD® (UPMCHealth Plan Payer ID: 23281)
- RelayHealth
- ALLScripts
Filing Method
- Electronic
(Prelog) – Allows direct submission of both professional (CMS-1500) and institutional (UB-04) claims via a user friendly interface.
- Paper Claim
CMS-1500 Form send to:
UPMC for YOU
P.O. Box 2995
Pittsburgh, PA 15230
CLAIM FILING
ORIGINAL CLAIMS
- 90 days after the date of service
RESUBMISSION OF DENIED CLAIMS
- 45 days of the initial submission
CLAIMS W/ THIRD PART LIABILITY
- Claim are received within 90 days of the primary EOB remittance date, or up to the new claim timely filling limit which ever is greater.
Appeal Rights
- 30 days after receiving denial from UPMC
- The appeal must be submitted in writing to UPMC at:
Provider Appeals
P.O. Box 2906
Pittsburgh, PA 15230 15230-2906
- UPMC will response after 5 days after receiving the appeal.
Contact Person
CHIP REYNOLDS
PHONE: 412-454-7260
EMAIL: Reynoldsgl@upmc.edu
PROVIDER: 866-918-1595 / 412-454-5664
EMAIL: CHCProviders@upmc.edu
AMERIHEALTH CARITAS
AMERIHEALTH
- Known as “the Plan”
- Is PA;s chc, MCO that will coordinate physical health care and long-term services and supports (LTSS) for older persons, persons with physical disabilities, and Pennsylvanians who are dually eligible for Medicare and Medicaid (Community Well Duals)
Recipients
- CHC Participants who are eligible and 21 yrs and older
- Who are dual eligible for Medicaid and Medicare
- Who are qualified for LTSS
How to Check Eligibility
- Verify a participant’s coverage with the plan by their plan identification number, social security number, name, birthdate or medical assistance identification number
- • Obtain the name and phone number of the Participant’s PCP
- Promise Visit www.promise.DHS.state.pa.us and click on PROMISe Online
MA HIPAA compliant PROMISe software (Provider Electronic Solutions Software) is available free-of-charge by downloading from the OMAP PROMISe website at:
www.promise.DHS.state.pa.us/ePROM/providersoftware/softwaredownloadform.asp
Prior Authorization
- Validity is 180 days or 6 months
- Any request in excess of 300 a month for diapers or pull-ups or a combination of both.
Fee Schedule
- 100% of PA Medicaid
Clearing Houses
- Change Healthcare
Filing Method
- Electronic
Electronic claims submitted without an NPI will be rejected back to the provider via their EDI clearinghouse. Network Providers who submit claims via paper CMS 1500 or UB-04 are also required to include their NPI on their claims
- Paper Claims
CMS-1500 Form send to:
Amerihealth Caritas PS CHC
Claims Processing Department
P.O. Box 7110
London, KY 40742-7110
CLAIM FILING
- ORIGINAL CLAIMS
180 days after the date of service
- RESUBMISSION OF DENIED and REJECTED CLAIMS
365 days of the initial submission for denied/ 180 days for rejected
- CLAIMS W/ THIRD PARTY LIABILITY
60 days of the date of the primary insurance EOB.
Appeal Rights
Claim submission is 365 days from date of service w/a written explanation of the error to:
AmeriHealth Caritas
Pennsylvania Community HealthChoices
Claims Disputes
P.O. Box 7110
London, KY 40742
For accurate and timely resolution of issues, Network Providers should include the following information:
Provider Name
Provider Number
Tax ID Number
Number of Claims involved
Claim numbers, as well as a sample of the Claim(s)
A description of the denial issue
All disputed claims will be acknowledged & decision will be conveyed within 60 days.
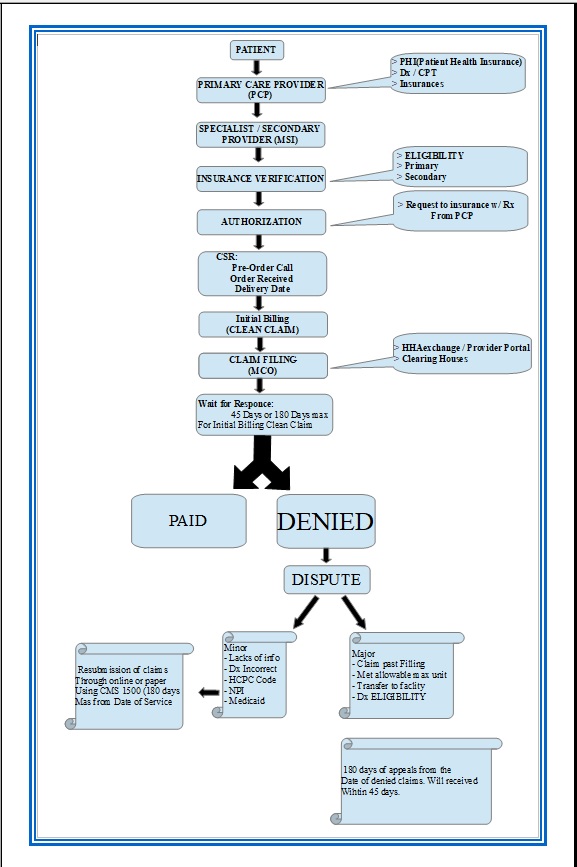
CHC – MCO Flow Chart