COMMUNITY HEALTHCHOICES (CHC) is Pennsylvania’s mandatory managed care program for individuals who are eligible for both Medicaid and Medicare (dual eligibles), older adults, and individuals with physical disabilities
CHC includes provisions to help maintain continuity of care and avoid interruptions of service for participants when they are first enrolled, as well as when choosing to switch from one managed care organization
(CHC-MCO) to another. Continuity of care also includes continuity of long-term services and supports (LTSS) providers. Each CHC-MCO must initially include in its networks all willing and qualified LTSS service providers
in the CHC-MCO service regions that are currently enrolled in the Medicaid program to provide home and community-based services in the Office of Long-Term Living (OLTL) waiver programs or nursing facility services.
This requirement will apply during the first 180 days of each phase of implementation.
NURSING FACILITY SERVICES
UPON IMPLEMENTATION
• If the CHC participant resides in a nursing facility in the CHC zone, the participant will be permitted to continue receiving care at that facility until he/she leaves the facility or is disenrolled from CHC, or if the facility drops out of the Medicaid program.
AFTER IMPLEMENTATION DATE
• Participants admitted to a facility after implementation will receive the standard 60-day continuity of care protections.
OTHER CONSIDERATIONS
• A change in CHC-MCO, a temporary hospitalization, or therapeutic leave does not interfere with or terminate the
continuity of care period as long as the participant remains a resident of the facility.
• The CHC-MCO in which the participant is enrolled must enter into an agreement with the nursing facility to make payments for care during the continuity of care period.
HOME AND COMMUNITY-BASED SERVICES
UPON IMPLEMENTATION
• For participants receiving home and community-based services
(HCBS) through a waiver program, the CHC-MCO must continue
providing care under the existing service plan using the participant’s
existing providers, including service coordination entities, for 180 days or until a comprehensive needs assessment is performed
and a person-centered service plan is created (whichever is later).
• During the first 180 days, if a participant transfers to a different CHCMCO,
the receiving CHC-MCO must provide previously authorized
services for: 1) the greater of 60 days or the remainder of the 180
days; or 2) until a comprehensive needs assessment is performed
and a person-centered service plan is created (whichever is later).
AFTER 180 DAYS
• If a participant transfers to a different CHC-MCO, the receiving CHCMCO must continue to provide previously authorized services for
60 days or until a comprehensive needs assessment is performed
and a person-centered service plan is created (whichever is later).
• If a participant chooses to transfer to a different CHC-MCO, service coordination will not be covered under the standard 60-day
continuity of care period, since service coordination will be viewed as an administrative function of the CHC-MCO.
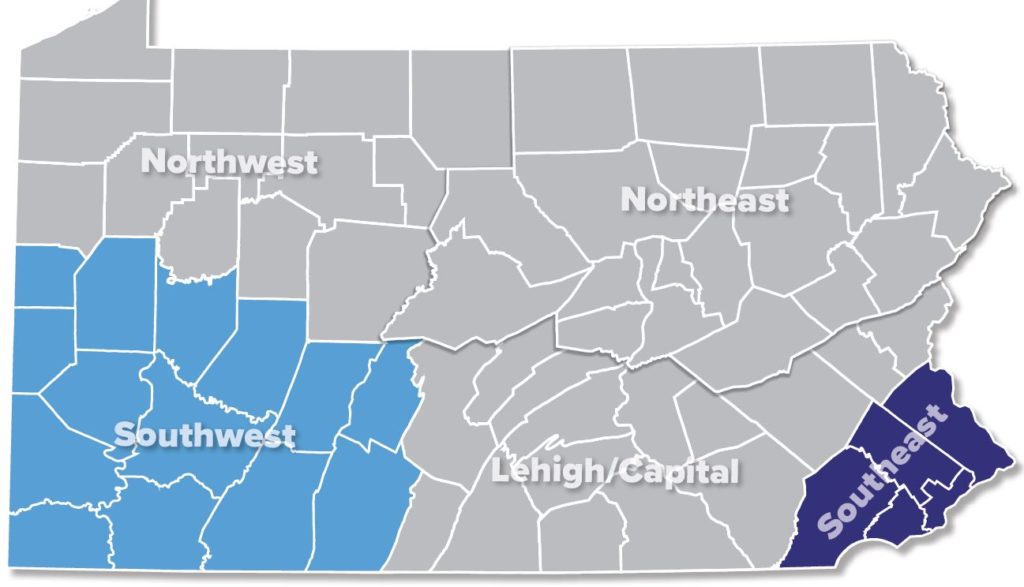
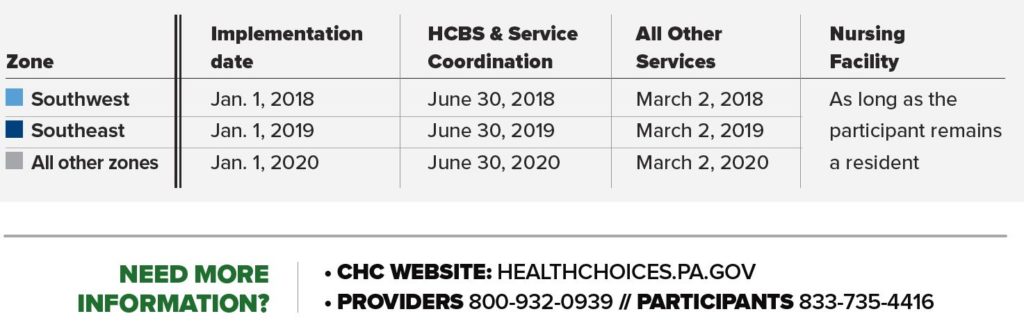
CHC IMPLEMENTATION DATE
Below are the initial continuity-of-care dates for CHC implementation. If a participant enrolls in CHC after the implementation date, all services will follow the standard continuity of care.