CLEAN CLAIM VS. UNCLEAN CLAIM
- Clean Claim – A clean medical claim is one that has no mistakes and can be processed without additional information from the provider or a third party.
- Unclean Claim – a claim that has been suspended in order to get more information from the provider.
REJECTED CLAIM VS. DENIED CLAIM
- Rejected Claim
- A rejected claim has been rejected because of errors. An insurance company might reject a claim because a medical billing specialist incorrectly input patient or insurance information.
- Once we received a rejected claim we can re-submit it for processing with an insurance company.
- Denied Claim
- A denied claim is one that has been determined by an insurance company to be unpayable.
- Claims are often denied because of common billing errors or missing information, but can also be denied based on patient coverage.
- Typically, insurance companies explain the reasons in the Explanation of Benefits (EOBs) attached to the claim.
- Denied claims have been received by the system of the insurance payor, and cannot be resubmitted because the payment determination has already been decided upon.
- Denied claims can be appealed and reprocessed in some cases. It can be appealed by the request of the payor to necessitate the proper modifications, additional required documents, etc.
WHAT IS MEDICAL BILLING APPEAL?
An appeal is a legal process where you are asking the insurance company to review it’s adverse benefit determination with the patient’s claim for benefits or you are appealing a provider contract issue.
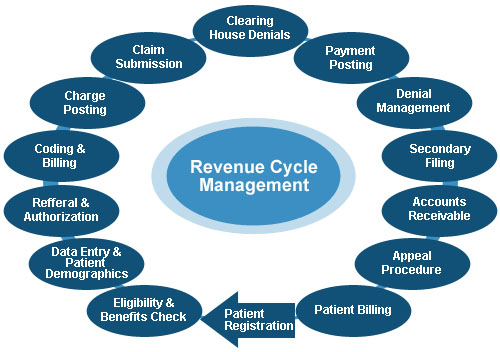
REVENUE CYCLE FLOWCHART