How to: View and Verify a Member’s Eligibility through the Provider Portal
The following information provides examples of various eligibility designations in the Provider Portal.
Log-In and Search Steps
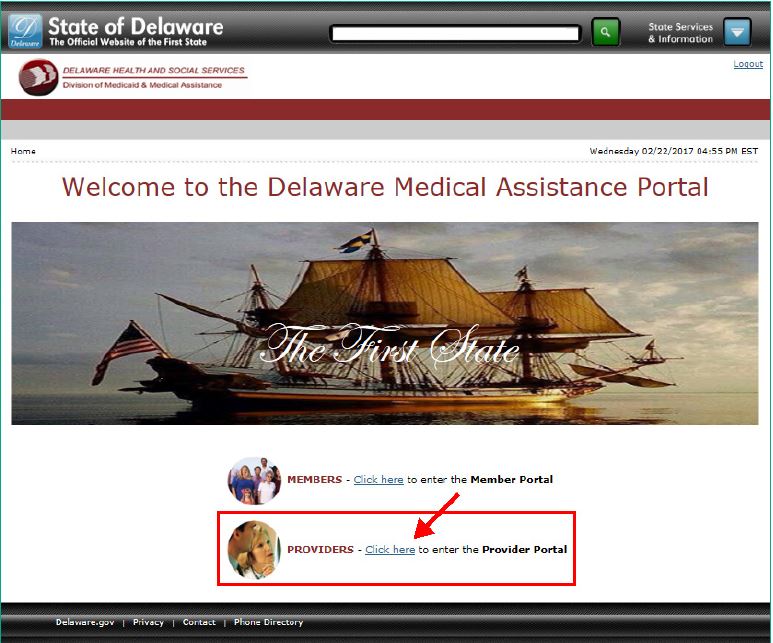
1. Go to the Delaware Medical Assistance Portal: https://medicaid.dhss.delaware.gov/.
2. Click here to enter the Provider Portal.
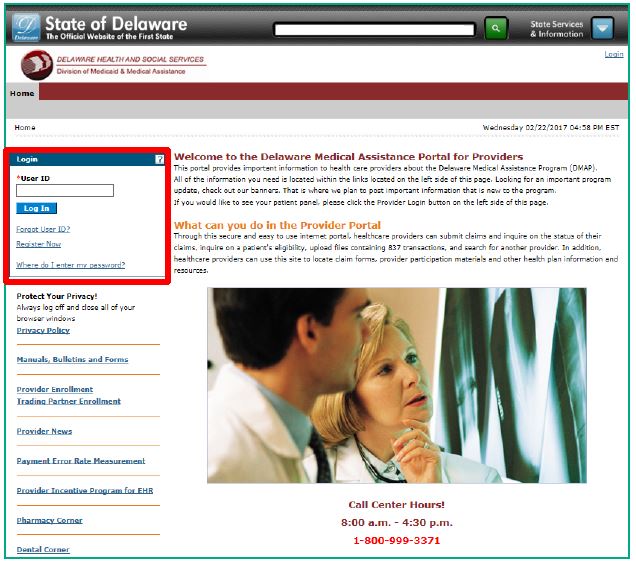
3. Log in by entering your User ID, Challenge Question, and Password.
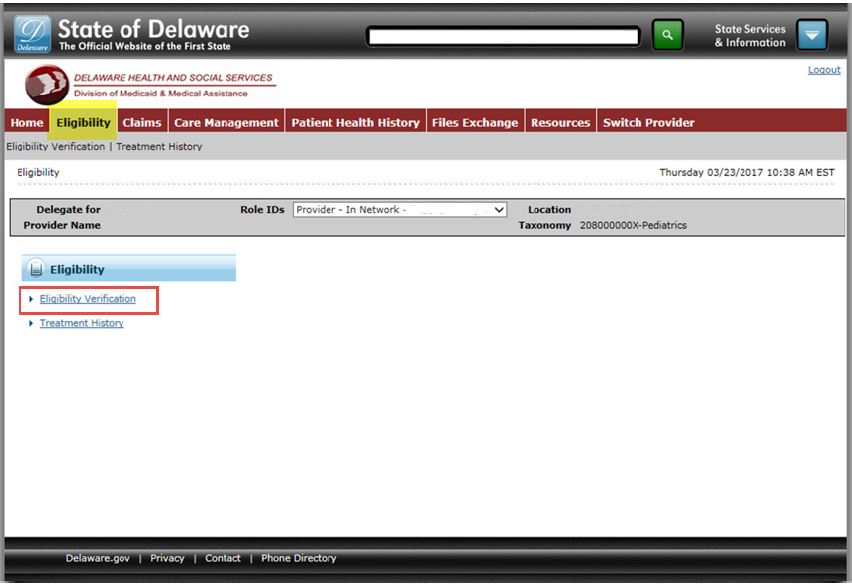
4. From the Home Page, click the Eligibility tab and then Eligibility Verification.
5. Perform a search for the member in the top portion of the page.
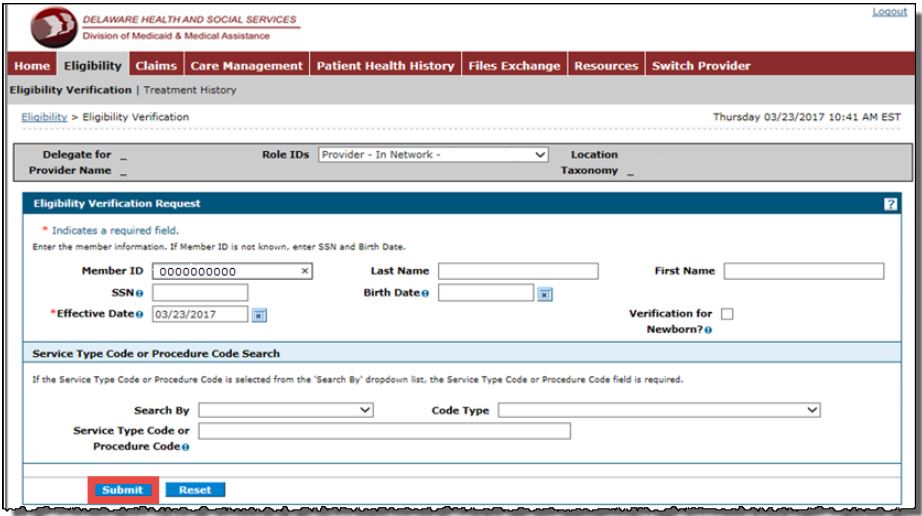
The bottom portion of the screen displays the search results with links to the Eligibility Verification Coverage (there can be more than one Coverage).
Eligibility Examples
The following describes the most common eligibility scenarios: QMB, SLMB, Illegal Non-Resident, DHCP (eligible), DHCP (ineligible).
Qualified Medicare Beneficiary (QMB)
1. Click the link, QUALIFIED MEDICARE BENEFICIARY.
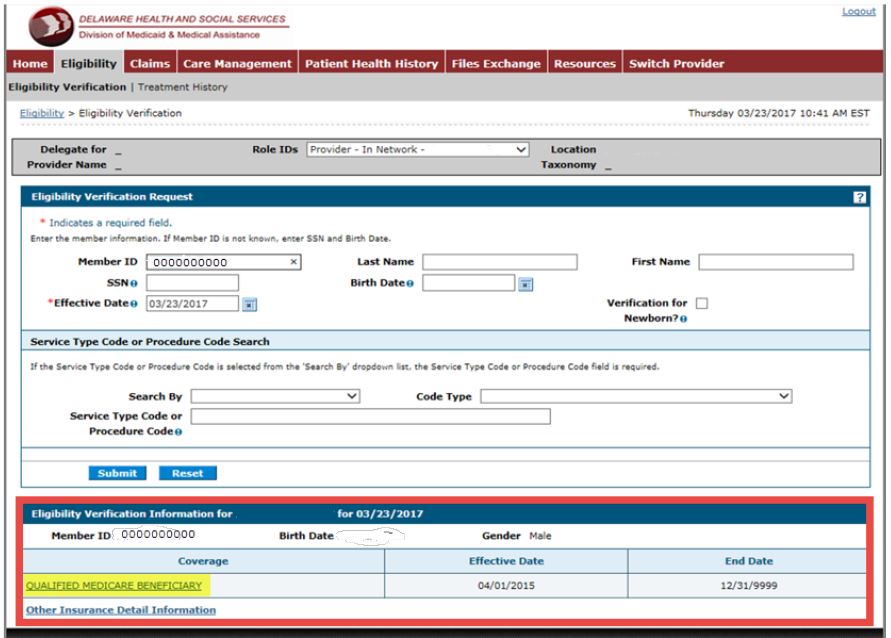
2. Review the Effective Date and End Date for the Coverage and Description listed.
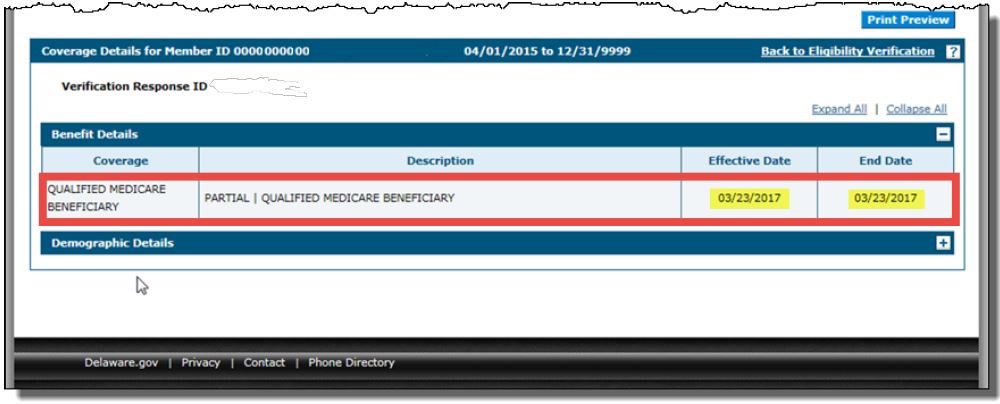
Note: Partial refers to a partial rather than a full Medicaid program/benefit. For coverage description/service covered, refer to the General Policy manual on the Provider Portal.
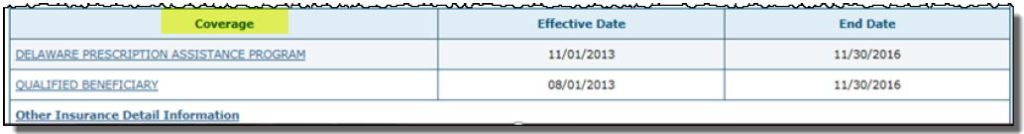
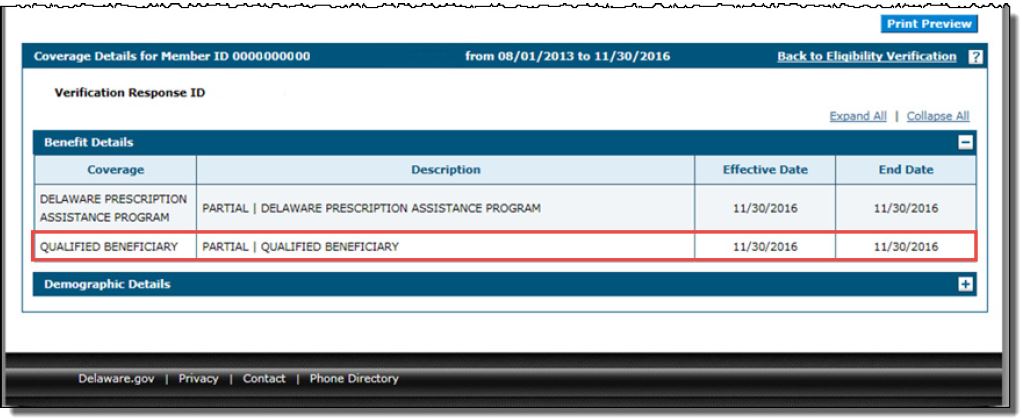
Specified Low-Income Medicare Beneficiary (SLMB)
1. Click the link, QUALIFIED BENEFICIARY.
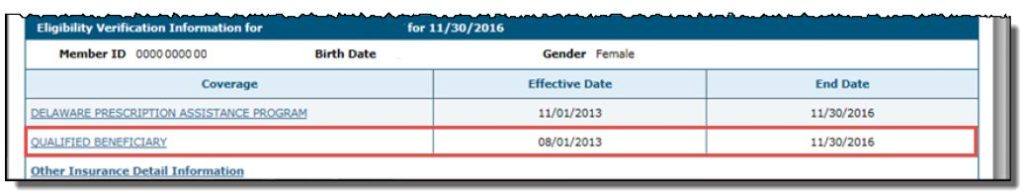
2. Review the Effective Date and End Date for the Coverage and Description listed.
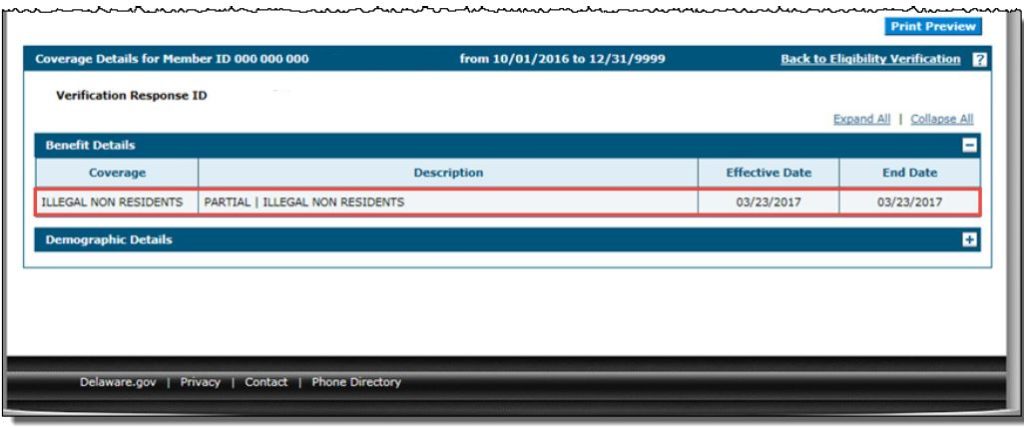
Illegal Non-Resident – Formerly Known as Emergency Service/Labor & Delivery
1. Click the link, ILLEGAL, NON-RESIDENTS.
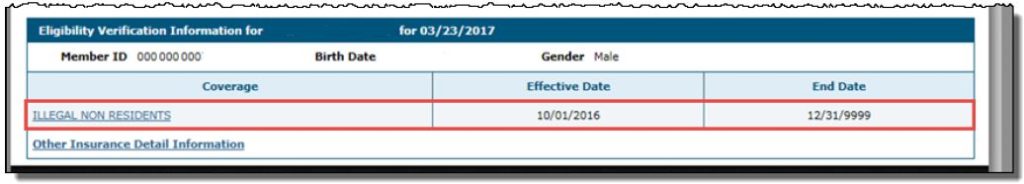
2. Review the Effective Date and End Date for the Coverage and Description listed.
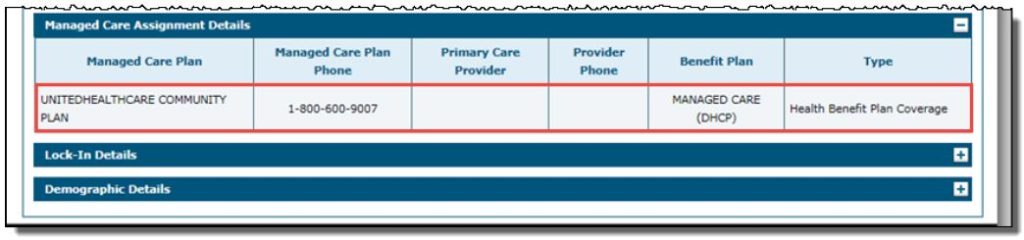
Delaware Healthy Children Program (DHCP) – Member IS ELIGIBLE for Date of Service
1. Click the link, DELAWARE HEALTHY CHILDRENS PROGRAM.
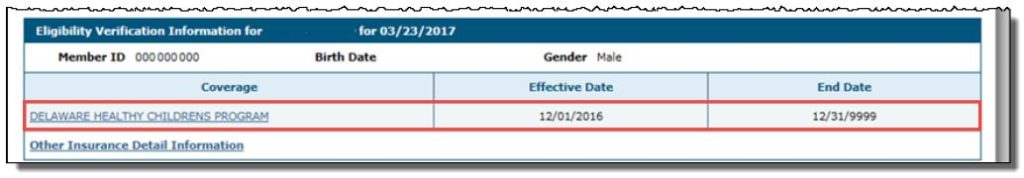
2. Review the Managed Care Assignment Details.
MPORTANT: There is a Managed Care Organization (MCO) assignment for the date of service (DOS); therefore, this member is eligible.
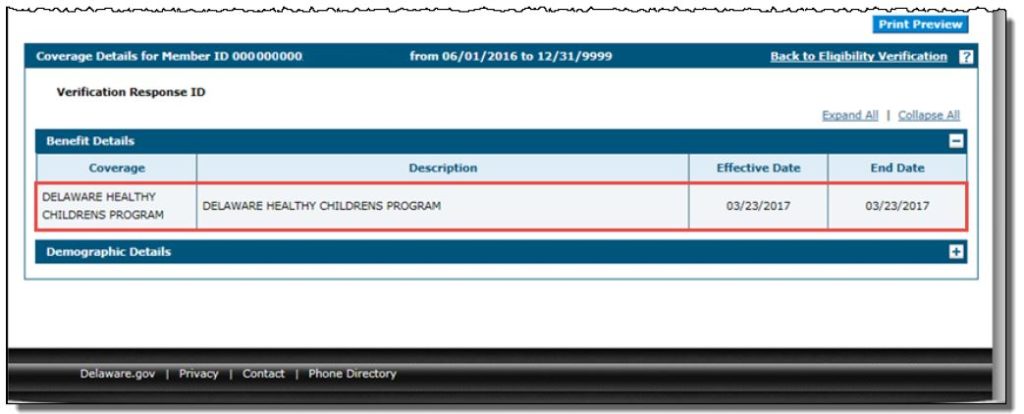
Delaware Healthy Children Program (DHCP) – Member Is NOT ELIGIBLE for Date of Service
1. Click the link, DELAWARE HEALTHY CHILDRENS PROGRAM.
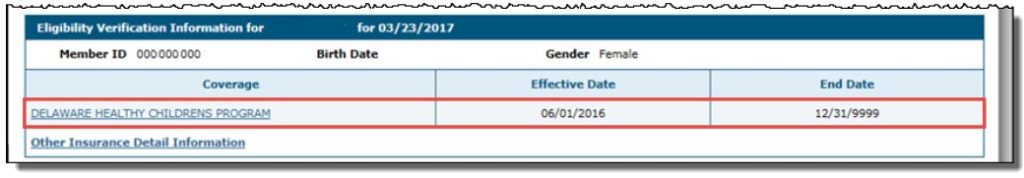
2. Review the Effective Date and End Date for the Coverage and Description listed.
IMPORTANT: There is no Managed Care Organization (MCO) assignment for the date of service (DOS); therefore, this member is not eligible.