MSI also processes billing of claims for supplies which are covered under the Waiver Program. Under this program, the federal government “waives” Medical Assistance/Medicaid rules for institutional care, giving our consumers the option to live independently in their own home and community. This benefit is extended to qualified members via service coordination entities and aging offices nearest the member’s residence. Here is where we get to meet the SCs and CMs.
Service Coordinators(SC) or Care Managers(CM) are representatives of the different aging agencies and service coordination entities all across the state of PA. These specialized people are assigned to every consumer and primarily responsible in maintaining individual care plans including the incontinence supplies and waiver items that MSI bills. SCs/CMs bring us potential consumers by selecting us as one of their qualified providers and also determine the continuity or cessation of consumer services, therefore greatly affecting our business.
All interactions with SCs/CMs regarding claims, whether by phone or email must be treated with the highest level of precision and accuracy. During inquiry, it is imperative that all details are ready in order to reduce the hassle of back and forth. Remember, SCs/CMs are always on the go, may not always have access to their office phone and emails and most importantly, they don’t like spending time addressing to non-issues.
GENERAL GUIDELINES
- Waiver items are allowed to bill only ONE TIME per month, because we only get paid ONCE per month.
- We cannot bill for two separate waiver claims under the same consumer within the same month. Doing so will make the first submitted claim PAID, then the second claim becomes DENIED. Therefore, we should not split sending of the waiver items.
- Sending of waiver items does not have to follow the Medicaid’s 31-day policy because it is the Waiver Program that pays for it. This means waiver items can be sent separately from the incontinence supplies. As long as the consumer receives the waiver items in any day of the authorized month specified in the service order, then the claim should be approved, unless there are technical difficulties, system issues or other situations beyond their control(e.g. the dates authorized on SO are not being picked up or not being translated from SAMS into HCSIS)
- SCs/CMs, upon their discretion, may setup sending of waiver items to consumers either Monthly, Every-Other-Month(EOM), or Every 3-months or Every 4-months. Whatever the setup, the goal is that the waiver items mustreach the consumer on the specified months authorized in the service order(SO). Otherwise, the claim may not be paid.
- Most aging office agencies utilize sliding dates when setting up service orders(meaning, we can bill them using a date of service anywhere from the 1st to the 31st day of the authorized month). Also, there are agencies(like the LANCASTER county) that use only a single date when we bill them, and that date must be consistent with the actual delivery date stated on the invoice that we send back to them(meaning, if we bill them using a date other than the actual delivery date stated on invoice, then the claim will not get paid because the dates will not match).
- Some SCs/CMs or service coordination agencies may request us to send them payment confirmation letters as a proof that the consumer supplies are getting paid by PA Medicaid. Please ask assistance from your Trainer or Lead on how to come up with a confirmation letter.
- SCs/CMs at any time, may request a copy of the consumer’s current script/RX covering the DOS of the denied claim in question. The purpose is to make sure that the doctor approves sending of waiver items. Remember, if the consumer has waiver items, we need to have both the service order and the RX intact before we can send out supplies.
- Some service coordination agencies use encrypted email(secured messaging) when sending out replies to claim inquiries. In this case, you may be prompted to create log-ins to their site in order to view the contents of the message. Agencies do this to implement HIPAA compliance so once you’re prompted, then you will have to continue the conversation using the encrypted platform.
SUGGESTIONS TO ENSURE CLAIMS ARE GETTING PAID:
- Split the delivery of incontinence supplies and waiver items as necessary. This is to make sure that consumers receive the waiver items according to the right months specified in the service order(SO).
- DO NOT SPLIT sending of the waiver items. wipesand creamsmust be sent together, all in one package so we can bill all waiver items under the same date of service(DOS).
- When logging service orders received from SCs/CMs, it is important that the person in charge of logging should accurately indicate the service start & end dates, the service frequency(if this is going to be monthly, every-other-month(EOM), or Every 3 months/4 months), the items to be sent, and the waiver total price. And, if at any point, there are details in the SO that don’t make sense, the person in charge should get back to the CM to clarify.
- For Service Orders setup for Every-Other-Month(EOM), or Every 3 Months/4 Months: This can be very tricky, and we may not know what we’ve missed until we start chasing the SCs/CMs for the denied claims. So to prevent this, we need to make sure that the authorized months are clearly indicated on the SO and properly logged in CSR workstation. This is important because the pattern that we have(based on the last delivery month) may not always be the same as what CMs have setup on their end, simply because they can just change/reset the months if they want(depending on the month they issue the new SO), so the existing pattern that we have may break.
- Always make the best efforts to resolve any inconsistencies in service orders. Not doing so may cause escalations from either the consumer or care managers, or non-payment of claims due to delivery errors which negatively impacts the billing. It may even lead to agencies pulling out from our service to look for another provider, which will greatly affect our business.
HOW DOES IT WORK?
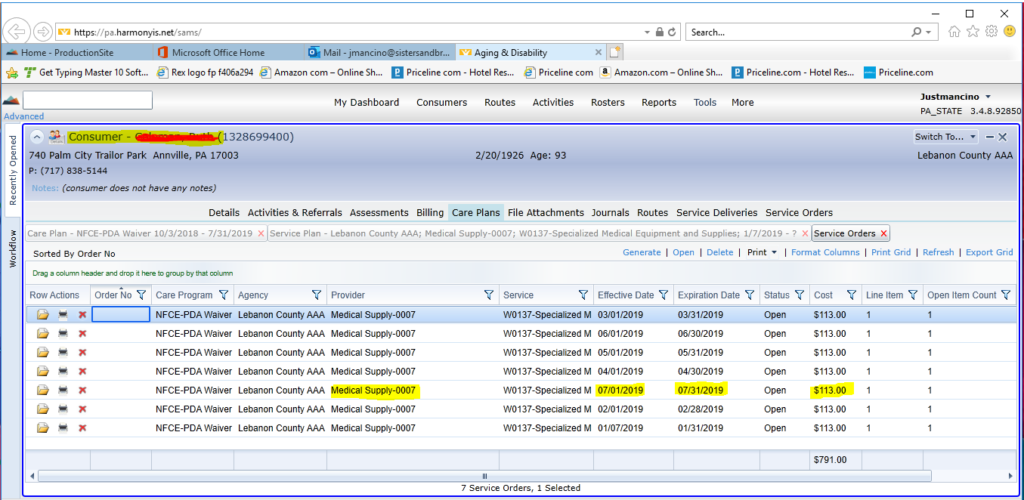
Below is the SAMS web-based system used by the SCs/CMs to enter and create service orders. This is how the service orders look like on the service coordination side. In this system, everything is laid out including the authorized provider, effective and expiration dates and the waiver approved monthly cost.
This below example of a consumer page is telling us that MSI is the listed provider for waiver items, we are authorized for monthly sending and we can bill anywhere from the first day to the last day of the month for a total monthly cost of $113.
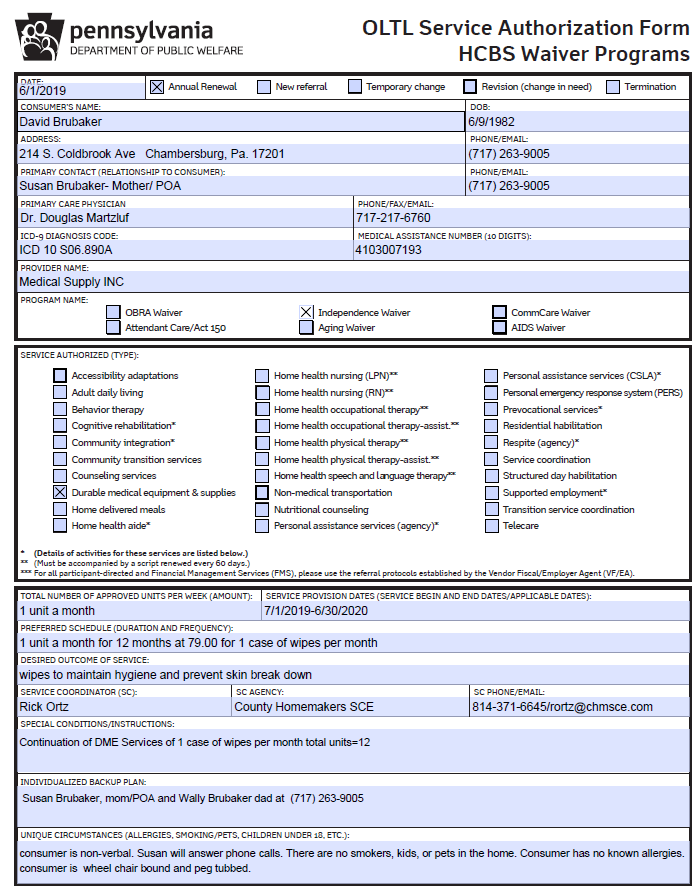
Along with creation of the service order in SAMS, the SC/CM also sends a copy of the same service order to MSI(via fax or email) in the form of a Service Authorization Form(SAF). This will serve as our reference and will be uploaded and logged under the consumer file. A sample copy of the SAF is provided on page 4.
Every instruction written in SAF has to be strictly followed to ensure payment of claims after delivery and most importantly, to avoid escalations from either the consumer or SCs/CMs.
After creating the service orders in SAMS, the information is then being translated into another system called HCSIS that stores and aligns the service order details to make it ready for billing. From SAMS, translation to HCSIS completes after at least 48-72 hours. Otherwise, refreshing/regenerating the service order usually does the trick so it will translate properly into HCSIS then claim finally gets paid.
If a claim gets denied even after billing it according to the service order, check the details of the claim. There might be other reasons that trigger the denial so we may need the help of the SCs/CMs. This is where the chasing and negotiations come in. A table of the most common claim statuses/denial reasons is available on page 10.
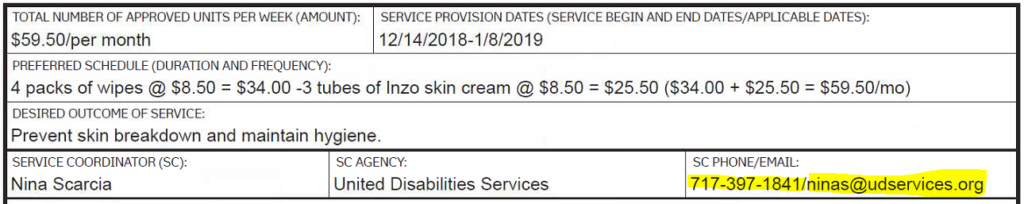
SAMPLE COPY OF A SERVICE ORDER
PAGE 1
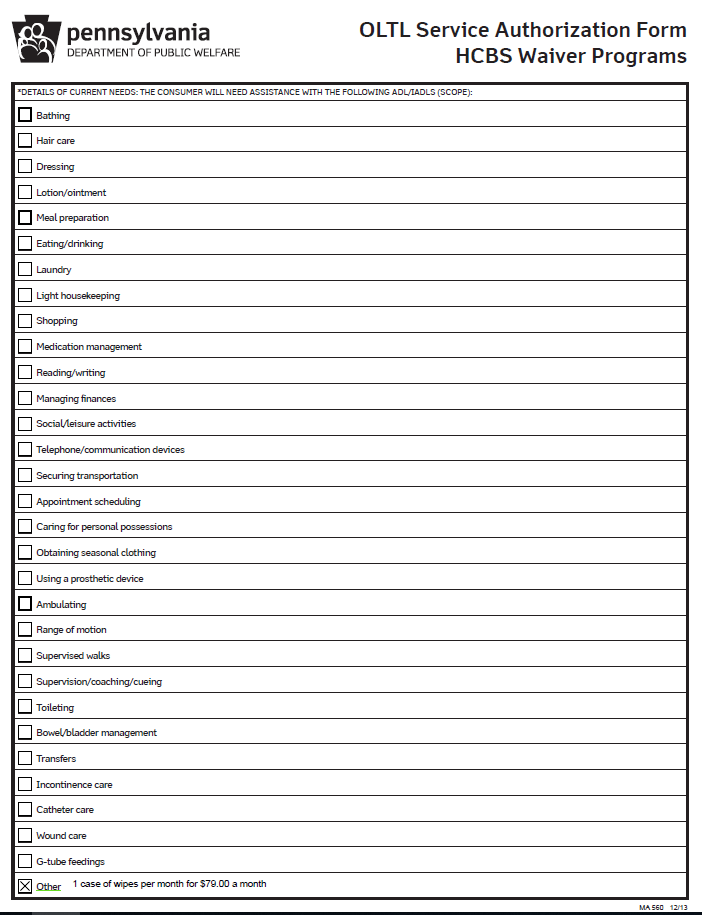
PAGE 2
CHECKING THE SERVICE ORDER IN ACCESS
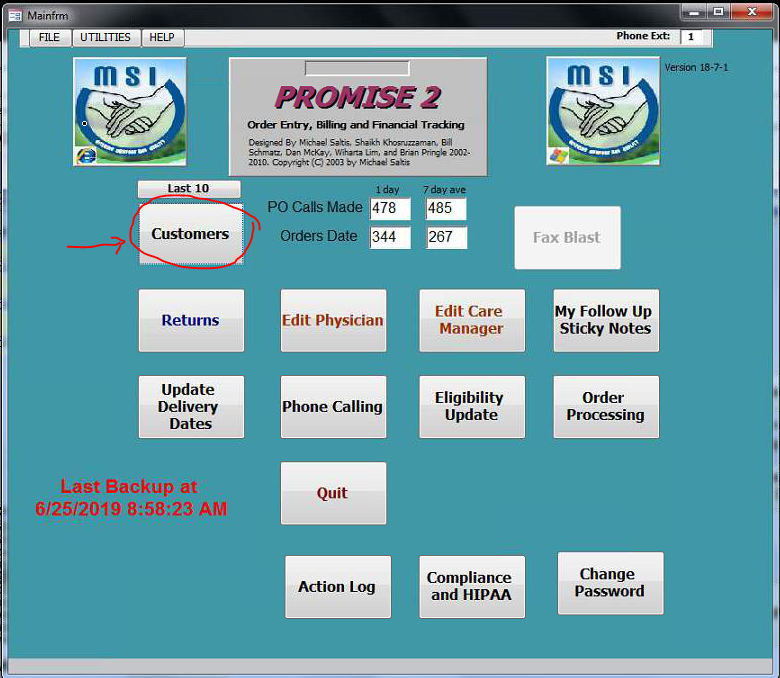
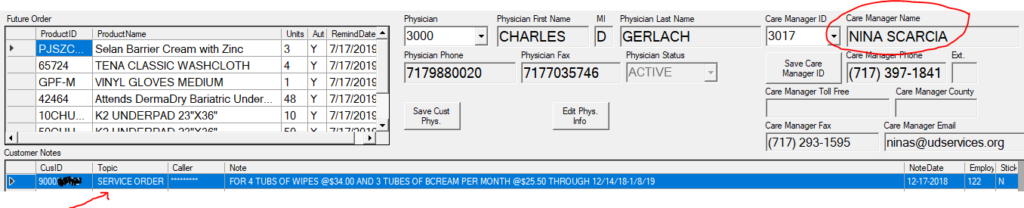
- Open the CSRWS in MS Access and login using your credentials. Click the Customers button, type a cons# and go to the selected cons customer page.
2. Go to the RX tab and you will be able to see the list of cons current RX Faxes and SO documents saved in PDF format. Highlight the applicable SO file then click the View Selected Fax or Document button and it will open the service order.
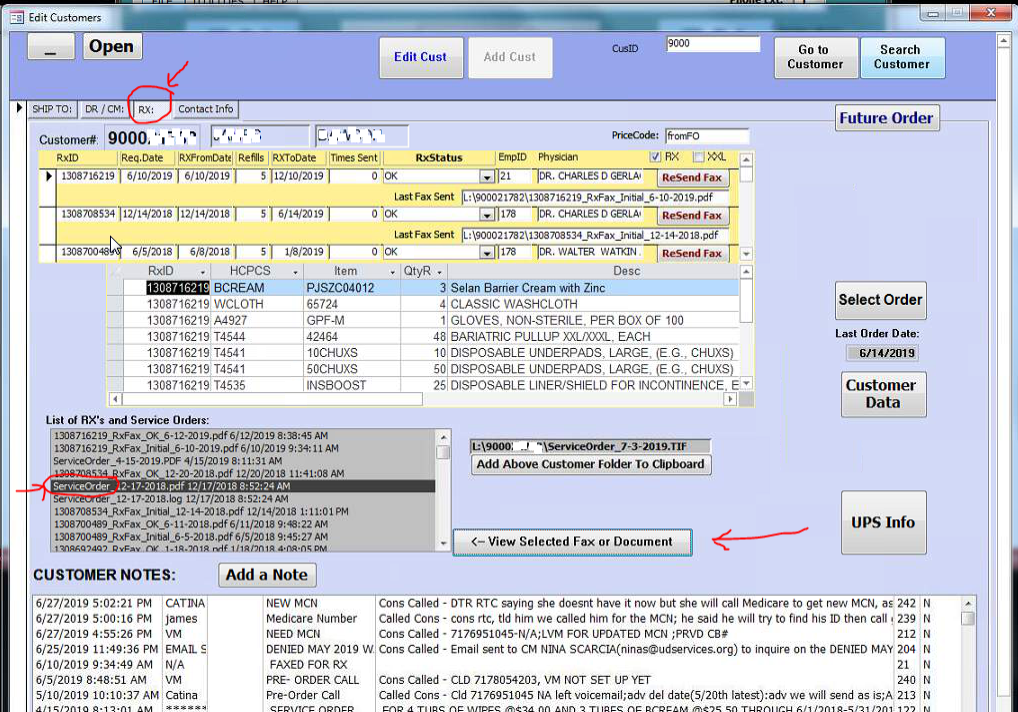
3. The Service Order shows the waiver service start & end dates, the service frequency(if this is going to be monthly, every-other-month(EOM), or Every 3 months/4 months), the items/number of units to be sent, the waiver price, and any special notes from the SC/CM.
The name of the SC/CM on the service order should be the same person listed in the CSRWS.
Service order should also be logged in the Customer Notes section of the CSRWS.
GETTING STARTED – PULLING UP WAIVER CLAIMS IN PROMISE
The goal in waiver billing is to make sure that all supplies sent to consumers are fully paid, no more, no less. In order to track this properly, it is strongly suggested to work on claims one month behind the current month (let’s say if this is the month of JULY, then we should work for the month of JUNE) to make sure that all claims are completely reported in Promise website and ready to be worked on. Most of the time, it takes at least 2-3 weeks to a month before the all claims get loaded and becomes available for viewing in Promise.
- Access the Promise website(with your credentials) and go to Claims tab. Make sure you’re on location 0007
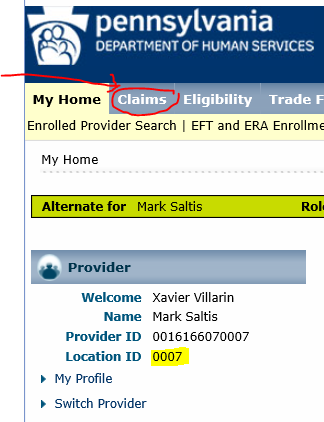
2. Populate the From Date using a single date of service. The same date can be used for the Thru Date. Click Submit button. A wider date range may be used but the number of results may be lengthy, so it is suggested to pull the claims using single dates until we reach the last day of the month.
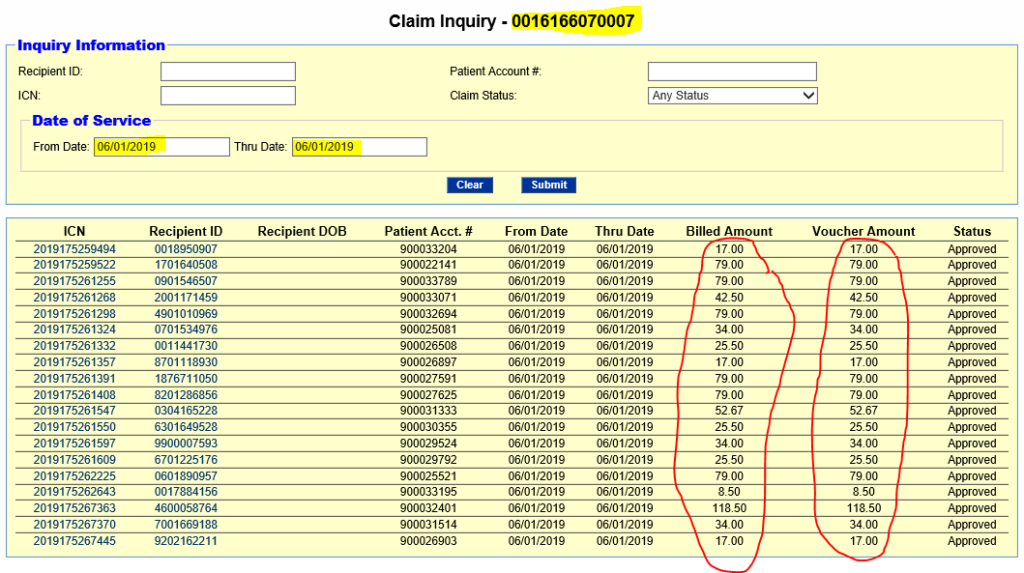
In this figure, we pulled all claims ranging from 06/01/2019 to 06/01/2019 so that we see all statuses of claims reported for that specific day. We check if the claims were paid/approved and then track down the claims that were denied. Ideally, the claims look good when we see them all approved with the billed amounts exactly matching the voucher amounts.
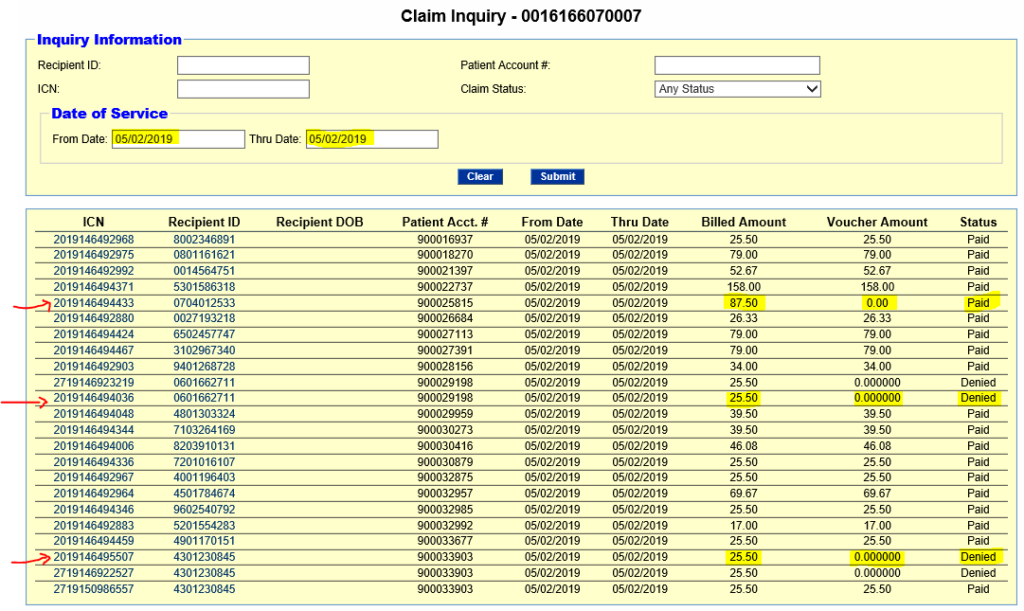
In this another example, we pulled the claims from 05/02/2019 to 05/02/2019 and now we see some denied claims and and a claim which was paid/approved but the voucher amount is at $0. When we explore other dates of service, it gets more interesting as we encounter more problematic claims with varying denial reasons. To find out the denial reason, click the ICN# on the left of the claim that you want to start working on.
3. Track the problematic claims starting from the 1stday to the 31st day of the month. It is suggested that we translate it into a workable spreadsheet/master list that can be updated and monitored until such time that problematic claims get paid/approved.
4. Once finished tracking the problematic claims for the whole month range, start establishing contacts with the service coordination entities and look for the assigned SCs/CMs. There might be other reasons triggering the denial so we may need their assistance to see what’s going on. This is where the chasing comes in. A table of the most common claim statuses/denial reasons is available on page 10.
5. If unable to get to SCs/CMs after several attempts, look for the service coordination supervisors. We get better answers if the supervisors come to rescue. There are also instances when we are directed to their billing department for help in fixing the claim. If still no luck, then go to the next higher support level. Remember, we need to get as much approved claims as possible, but if they have to deny a claim, then we have to validate why.
6. It is advisable to maintain a directory of phone numbers and emails of the SCs/CMs/Supervisors of the different service coordination agencies you’ve previously worked with. This will be a big help if you need to get answers in case another SC/CM is not reachable.
TROUBLESHOOTING ISSUES WITH APPROVED/DENIED WAIVER CLAIMS:
It’s nice to see claims getting approved, because this means money. But once we start getting denied claims, then we start losing money. This is where your analytical thinking, thorough investigation and negotiation takes place. Fixing denied claims would require lots of creative approaches and professionalism because this is where the chasing of service coordination comes in.
Take note that the person in charge of PA waiver billing will interact directly with SCs/CMs and service coordination entities with varying standards in setting up service orders. They may also have varying policies and requirements in resubmitting denied claims. Remember, as previously mentioned, the SCs/CMs are always on the go, may not always have access to their office phone and emails and most importantly, they don’t like spending much time addressing to non-issues, so please be very careful every time you initiate a claim inquiry. Escalations can go from care managers up to service coordination supervisors, and even to as high as service coordination presidents and operation directors.
The table below lists the most common claim statuses/denial reasons and their corresponding definitions. You will also find the suggested steps that can be done to help fix the claim.
| CLAIM STATUS / DENIAL REASON | DEFINITION | WHAT TO DO? |
| PAID/APPROVED | Claim already paid and should be in full amount. | No more action required because claim is already paid in full. |
| RATE APPROVED LESSTHAN BILLED | Claim is paid but less than the amount that we billed for. | *Verify the right amount that should be billed for. *Ask SC/CM to correct the pricing setup on their end using the SAMS System; then request to regenerate the service order so the corrections will translate to HCSIS. |
| SERVICE INDICATED, BUT NO UNITS AVAILABLE IN HCSIS | A claim has been previously paid but there’s another claim being submitted again for the same month, causing the denial. | *Check if there’s another claim submitted for the same month; if YES, then first claim will be PAID and the second claim will be DENIED; we only get paid ONCE a month. *If NO, then verify with SC/CM if there is a service order entered for the consumer. *Request SC/CM to regenerate the service order so the corrections will translate to HCSIS. |
| BEGIN DOS INVALID IN HCSIS | *Possibly no service orders entered for the consumer. *Possibly the consumer transferred to another county or another state *Possibly the date of service does not match with the date setup by the SC/CM | *Verify with SC/CM if there is a service order entered for the consumer *Verify if the SC/CM is using sliding dates or just a single date when setting up service order. *Request SC/CM to regenerate the service order so the corrections will translate to HCSIS. |
| PROCEDURE INVALID IN HCSIS | *Possibly no service orders entered yet for the consumer. *Possibly the consumer transferred to another county or another state | *Verify with SC/CM if there is a service order entered for the consumer *Request SC/CM to regenerate the service order so the corrections will translate to HCSIS. |
| PROVIDER ID INVALID IN HCSIS | *Possibly no service orders entered yet for the consumer. *Possibly the consumer transferred to another county or another state *Possibly we are not the qualified provider listed on the system by SC/CM | *Verify with SC/CM if there is a service order entered for the consumer *Request SC/CM to regenerate the service order so the corrections will translate to HCSIS. |
| RECIPIENT NOT ELIGIBLE FOR SERVICE PROVIDED RECIPIENT ELIG EFF DT > THE DOS ON THE CLAIM | *Possible eligibility lapses. *The DOS came before the consumer’s date of eligibility. | *Run ELIGIBILITY check to verify if consumer is covered on the DOS. *Verify with SC/CM if there is a service order entered for the consumer |
| RECIPIENT NOT ELIGIBLE FOR SERVICE PROVIDED RECIPIENT INELIGIBLE ON DATE(S) OF SERVICE | *Possibly the consumer was NOT ELIGIBLE by the time the waiver items were delivered. *Possibly the consumer transferred to another county or another state | *Run ELIGIBILITY check to verify if consumer is covered on the DOS. *Verify with SC/CM if there is a service order entered for the consumer |
| RECIPIENT CHC COVERED ON DATE OF SERVICE | Claim will be DENIED because CHC will pay for the waiver items. | No more action required. |
| DATE OF DEATH IS PRIOR TO DATE OF SERVICE | Consumer was reported DECEASED before the waiver items were delivered | *Place a note in CSRWS; update hold code to DECEASED; term insurances and request to pull out the file |