HEALTHCHOICES is Pennsylvania’s mandatory managed care program for 2.2 million Medical Assistance participants. Participants receive quality medical care and timely access to all appropriate physical and behavioral health services and/or drug and alcohol services.
COMMUNITY HEALTHCHOICES (CHC) is Pennsylvania’s mandatory managed care for dual-eligible
individuals and individuals with physical disabilities — serving more people in communities rather than
in facilities, giving them the opportunity to work, spend more time with their families, and experience an
overall better quality of life. When implemented, CHC will improve services for hundreds of thousands of
Pennsylvanians, including older Pennsylvanians and individuals with disabilities.
WHAT IS SIMILAR?
• Both are Medicaid Managed Care Programs:
Both programs utilize managed care organizations
(MCOs) to provide coverage for their members.
The commonwealth pays the MCOs a capitated
monthly rate (like a premium for each member),
and the MCOs coordinate the health care needs
for their members.
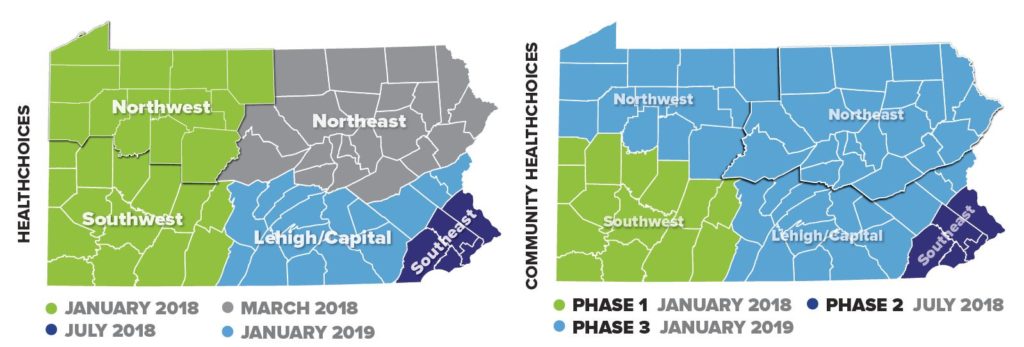
• Zones: HealthChoices and CHC use the same
five geographic zones.
• Choice: Members of both plans choose their MCOs.
• Physical health benefits: HealthChoices and
CHC both offer the Adult Benefit Package for
physical health services.
• Behavioral health benefits: Both HealthChoices and
CHC are required to coordinate participants’ behavioral
health services from the Behavioral HealthChoices MCOs.
WHAT IS DIFFERENT?
• Dual-eligible coverage: CHC provides coverage for
participants who are eligible for both Medicare and
Medicaid. This means that the CHC-MCOs will have
to coordinate closely with Medicare to ensure that
participants have access to comprehensive services.
Also, CHC-MCOs will have the ability to provide
Medicare coverage (called D-SNPs) to participants
who would like their Medicaid and Medicare services
coordinated by the same entity.
• Long-Term Services and Supports (LTSS):
CHC provides LTSS to participants who need the level of
care provided in a nursing home. Participants who meet
this criteria will receive LTSS services and physical health
services from their CHC-MCO, including nursing facility
care. HealthChoices MCOs will cover the first 30 days of
nursing facility care. If a participant continues to need that
level of care, the participant will apply for CHC.
ELIGIBILITY
Eligibility requirements for each program varies. The chart below
shows, in general, which program individuals might qualify for.
• Children up to, and including, 20 years old
• Adults
• Pregnant women
• Some women with breast and/or cervical cancer
• Lawfully present immigrants might be eligible
• Individuals ages 21 and older who are dually eligible
for Medicare and Medicaid
• Individuals ages 21 and older who need the level of care
provided by a nursing facility
• Individuals with intellectual or developmental
disabilities who are eligible for services through the
Office of Developmental Programs and residents
of a state-operated nursing facility (including state
veterans’ homes) are not part of CHC
SELECTING A PLAN
CHC is a new program slated
for a phased implementation in
January 2018, while HealthChoices
has been available for over 20 years.
Everyone going into CHC will need to
select a plan. For HealthChoices, some
participants will have to select a new
plan because their plan may no longer
be available in their area. Everyone in
HealthChoices, will be given the option
of switching plans, if desired.
MCOs IN EACH ZONE
A competitive procurement was
completed for both HealthChoices
and CHC. For CHC, three MCOs will be
available for participants in each zone:
· AmeriHealth Caritas
· Pennsylvania Health
and Wellness (Centene)
· UPMC for You
For HealthChoices, an announcement was made about newly selected MCOs.
The current MCOs remain in place, and an announcement will be made at a later date concerning the newly selected MCOs.
TIMELINES FOR IMPLEMENTATION To ensure a successful transition,
the same implementation timeline will be used for both HealthChoices and CHC, with a few exceptions: