PA/MA WEBSITE BILLING
STEP 1: Copy and paste MA SERVICE PRGRSM ID RECP NO to RECIPIENT ID on CLAIM INQUIRY PAGE. Put in Service Dates.
See Diagram 2 for instructions.
DIAGRAM 1:
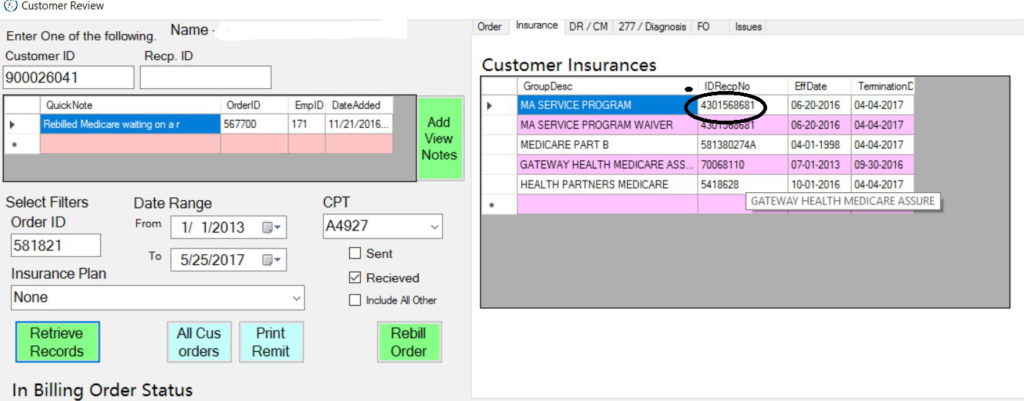
DIAGRAM 2:
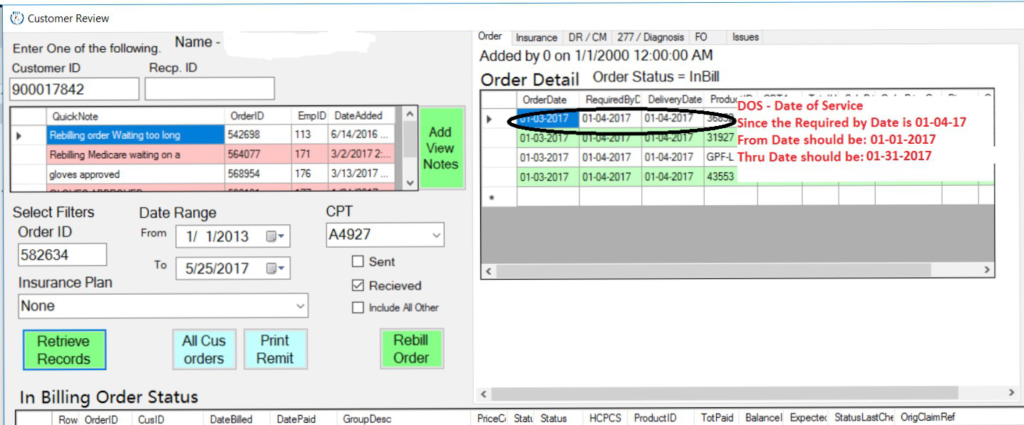
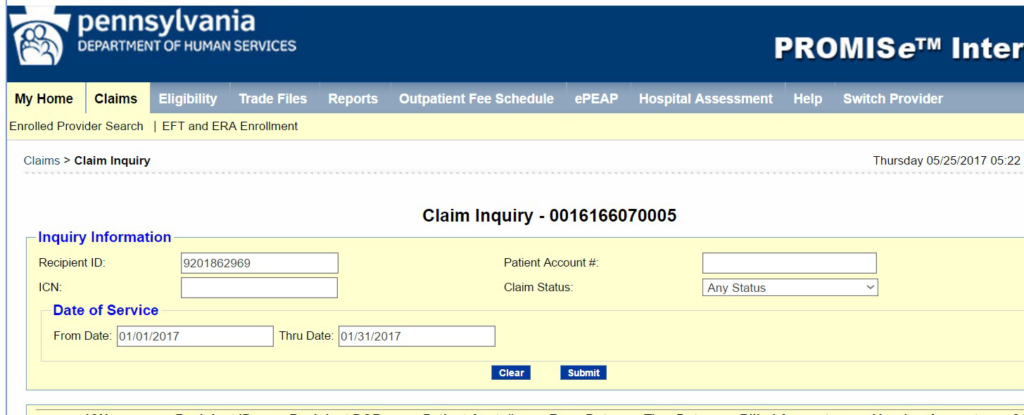
DIAGRAM 3: The PA/MA Claim Inquiry page is where you paste all the information you have gathered in Diagrams 1 and 2.
STEP 2: Once you see the Claim Reference numbers in the Claim Inquiry Page, check first the Denied Claim Reference number. Match the Denial found with the Denied Claim Reference number. If in one of the details says Denied and it says that the Patient has PVT INS or NO Denial Indicated (see 2nd picture). Most of the time we would need to check the service adjustments on the denied claim. (see continuation after diagrams)
DIAGRAM 1:
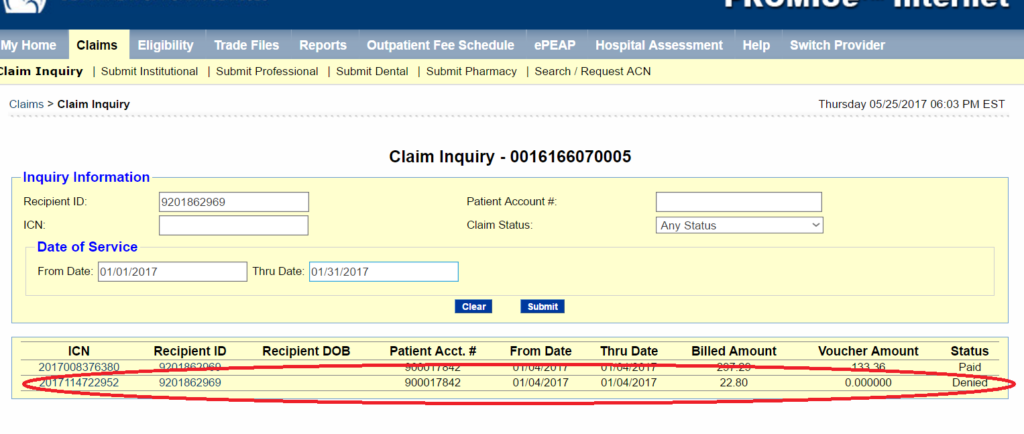
DIAGRAM 2:
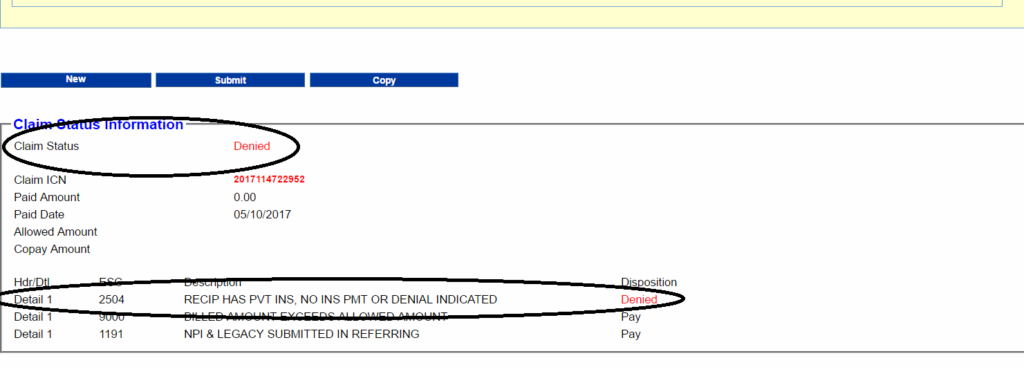
DIAGRAM 3:
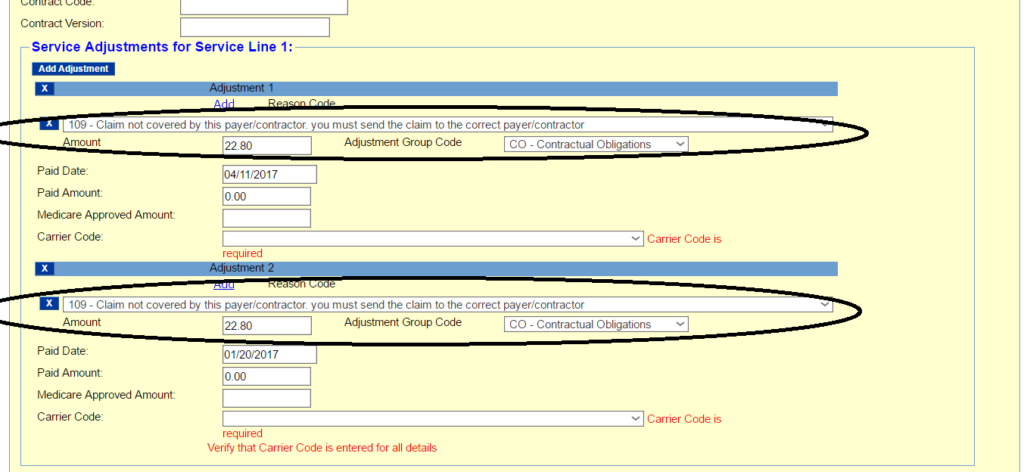
DIAGRAM 4:
This claim has been denied because the service adjustments for the gloves line is incorrect. On DIAGRAM 3, the Adjustment 1 on the First Service Line is: ADJUSTMENT REASON CO-109, Amount Group Code is CO or Contractual Obligations, amount is $22.80, PAID DATE is 01/20/2017 – where can you get this date? (you can get this date from the IN SENT RECEIVED SECTION of the BILLING WORKSTATION under CREATE DATE that matches NORIDIAN)
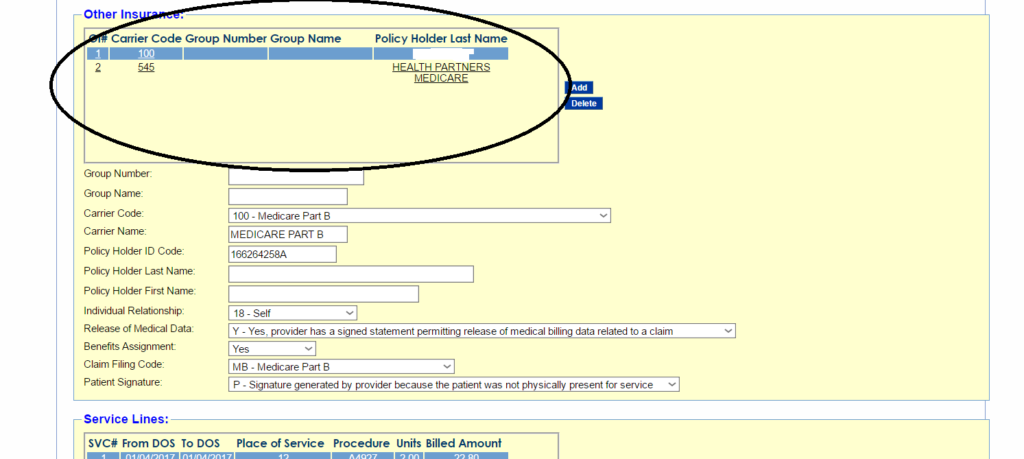
(in other instances, the claim will also be denied if it doesn’t have the right insurance Carrier Name, a good example will be a Cigna Medicare Advantage – we get good number of denials from Cigna Medicare Advantage because the Carrier Code for Cigna is 542 in PA MA but the Code where CIGNA Medicare Advantage would get approved is Carrier Code 516 which is Bravo in PA MA)
*** TYPICALLY, we do not work on DENIED CLAIMS, however, if the denied claim for the gloves is less than 6 months form the date of service, we can still reprocess the claim as an ORIGINAL CLAIM.