PROCESSING A DENIED CLAIM AS AN ORIGINAL CLAIM
STEP 1: Copy the CLAIM REFERENCE NUMBER at the bottom of the PROFESSIONAL CLAIM PAGE in the CLAIM STATUS INFORMATION SECTION.
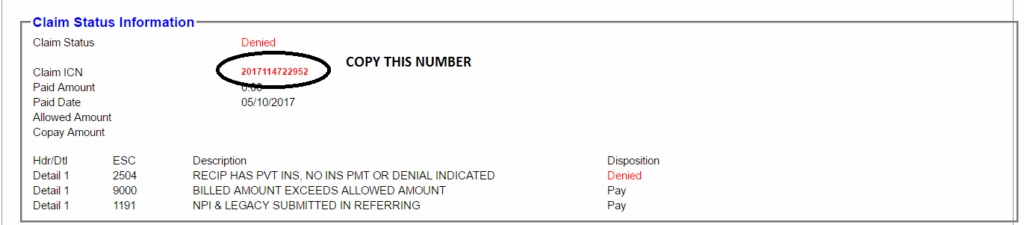
*** look at the paid date detail, if the paid date detail is less than 65 months from the Date of Service you can definitely process this as an original claim.
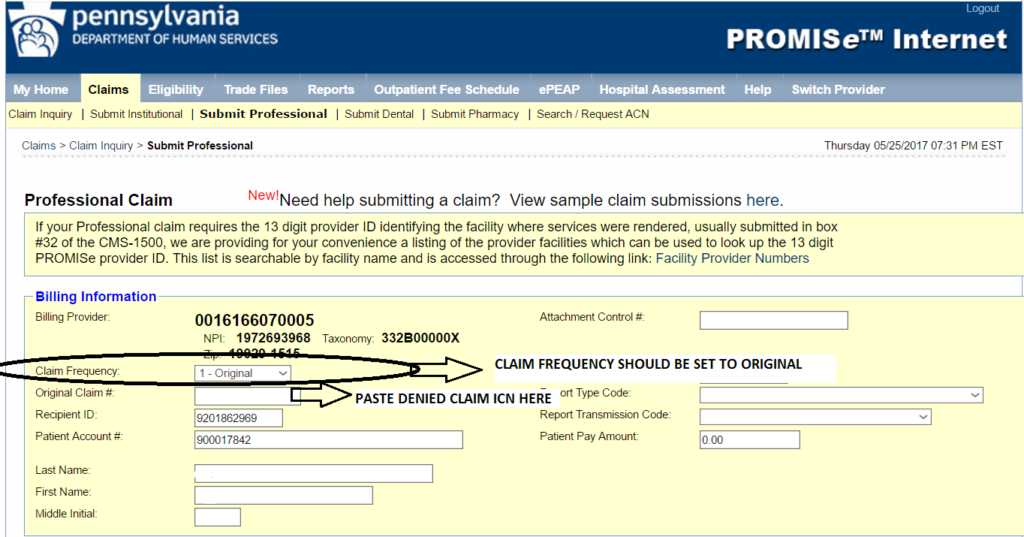
STEP 2: Paste the copied CLAIM ICN to the original CLAIM NUMBER FIELD in the BILLING INFORMATION SECTION. CLAIM FREQUENCY should be set to 1-ORIGINAL.
STEP3: Fill in all necessary information on other insurance section: Click ADD, Do MEDICARE PART B first. Copy MEDICARE PART B RECIPIENT ID NUMBER in BILLING WORKSTATION under INSURANCE TAB. Make sure that all details are correct.
If the patient has another INSURANCE PROVIDER (a COMMERCIAL INSURANCE). Click ADD After putting in the MEDICARE PART B. INFORMATION Click ADD, Then fill out the other details on the other INSURANCE TAB. in this scenario, the patient has another insurance, which is HEALTH PARTNERS MEDICARE, in the CARRIER CODE FIELD scroll down to NUMBER 545 – which is the CARRIER CODE for the HEALTH PARTNERS MEDICARE. Fill in POLICY HOLDER ID, INDIVIDUAL RELATIONSHIP, RELEASE OF MEDICAL DATE, BENEFIT DATE, BENEFIT ASSIGNMENT, CLAIM FILING CODE, PATIENT SIGNATURE.
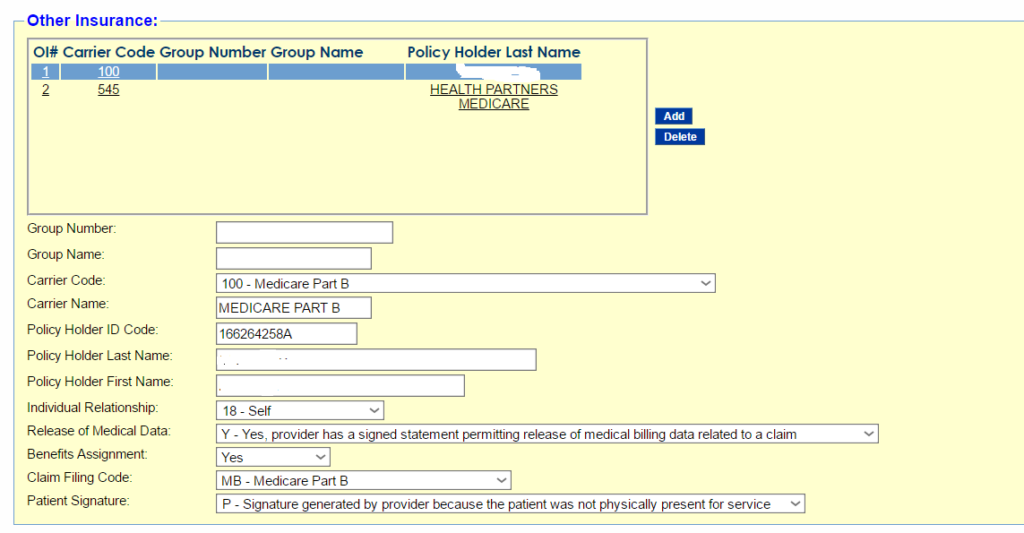
FOLLOW THE CODES for EACH FIELD
EXAMPLE:
INDIVIDUAL RELATIONSHIP: 18 – SELF
RELEASE OF MEDICAL DATE: Y – Yes, provider has signed statement permitting release of medical billing date related to a claim.
BENEFIT ASSIGNMENT: Yes
CLAIM FILING CODE: MB- Medicare Part B
PATIENT SIGNATURE: P – Signature generated by provider because the patient was not physically present for service.
STEP 4: Fill out the SERVICE LINE PART OF THE CLAIM. FORM DOS – Date of SERVICE AND TO DOS should be identical dates. PLACE OF SERVICE: 12 HOME, PROCEDURE: Fill in the correct HCPC CODE, in this case A4927.
Be sure to fill in the following fields:
DIAGNOSIS POINTER: 1
BASIS of MEASUREMENT: UN
UNITS: 1 or 2 – depending on how many boxes the px gets per month
BILLED AMOUNT: 1 1 box – $11.40/ 2 boxes – $22.80
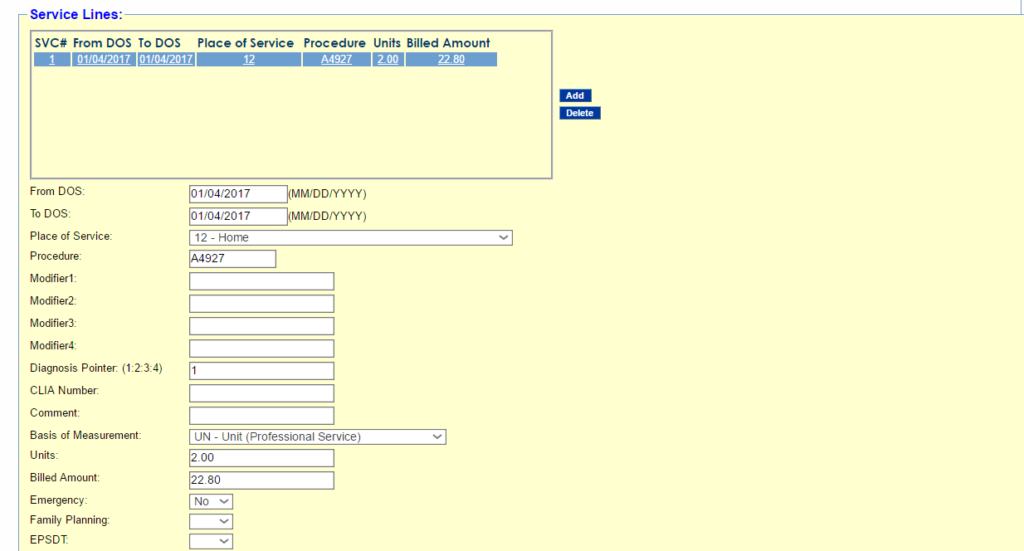
Once every field hat needs to be filled out in the Service Lines Portion are filled out proceed to STEP 5.
STEP5: THE SERVICE ADJUSTMENT/S PORTION. Click on ADD ADJUSTMENT, this is the Blue Button on the left upper part of the Service Adjustment portion. Put in the Reason Code- 109 Claim not covered by this payer/contractor you must send the claim to the correct payer/contractor. Amount id $22.80, Adjustment Group Code is: CO-Contractual Obligations. Paid Date: See Diagram 2 of step 5 where to find the paid date in the Customer Review Window. Paid Amount is zero because the claim is not professional Claim. SEE DIAGRAM, BELOW.
DIAGRAM 1:
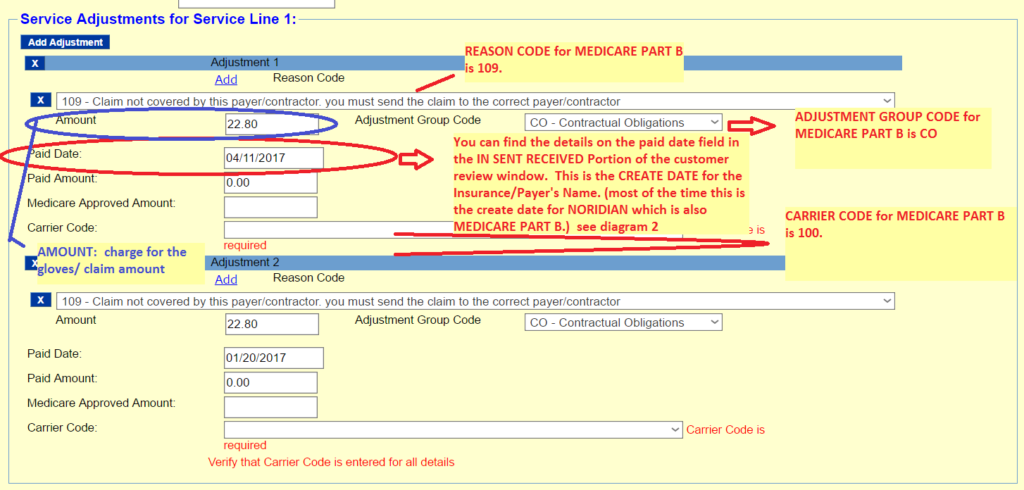
In this diagram the paid date on the service line adjustment is wrong, the correct PAID DATE should be 01-20-2017. SEE DIAGRAM 2.
DIAGRAM 2:
Please refer to instruction above.
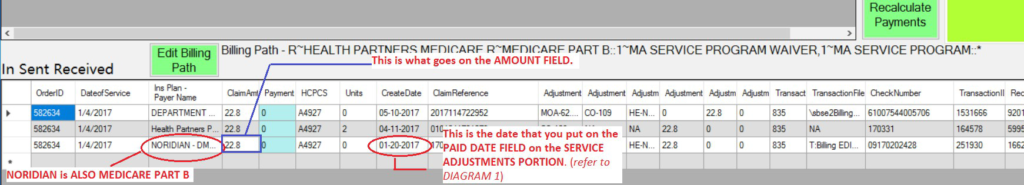
STEP 6: (for customer who have more than just PA Medicaid and MEDICARE PART B or have additional COMMERCIAL INSURANCE) CLICK on Add Adjustment again, then on the 2nd adjustment, scroll down to Reason Code 50-Non Covered Services. Put in $22.80 as amount or the amount of the Claim in In Sent Received, Paid Date Should be equal to the Create Date for the Commercial Insurance as shown on the diagram above. (SEE DIAGRAM 2 of Step 5) Put in CARRIER CODE (in this case, the CARRIER CODE for HEALTH PARTNERS MEDICARE is 545), scroll down to 545 or type the number. When you have filled out all the necessary fields, check the whole page for any RED MARKS – this means missing or incorrect information and then CLICK on SUBMIT.
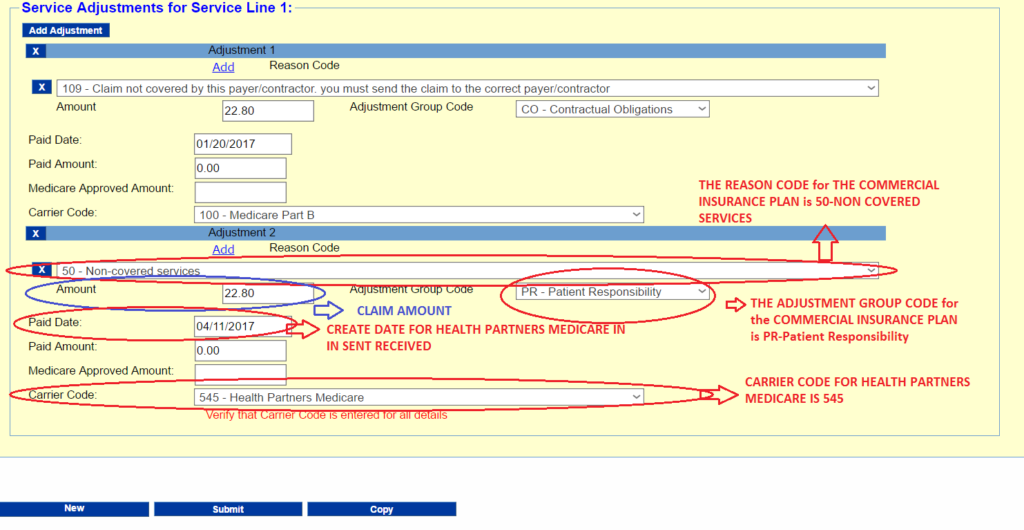
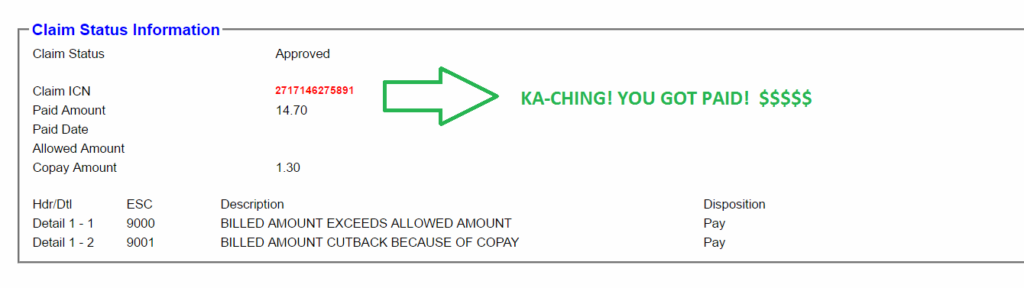
Click this part of the page to submit the
claim and if every information that you
keyed in, you should get this after the
star stops dancing.
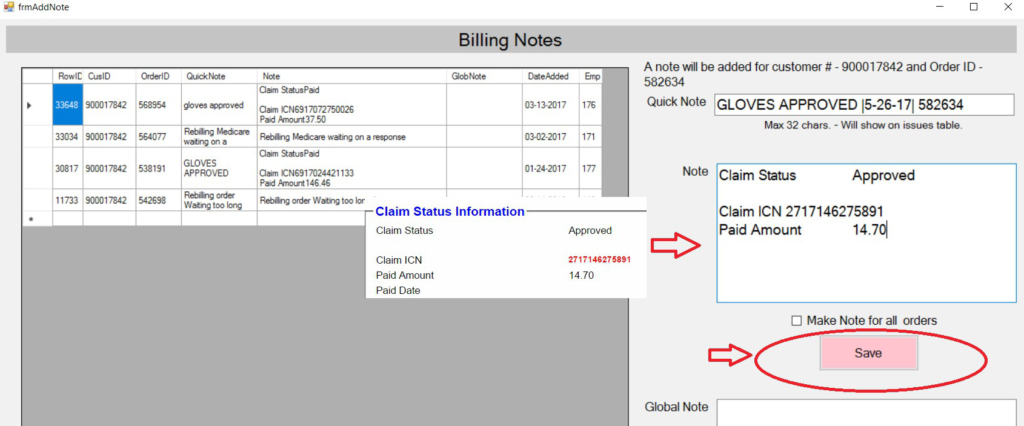
STEP 7: Copy and paste the NOTES ON THE CLAIM STATUS INFORMATION BOX as shown on the IMAGES BELOW:
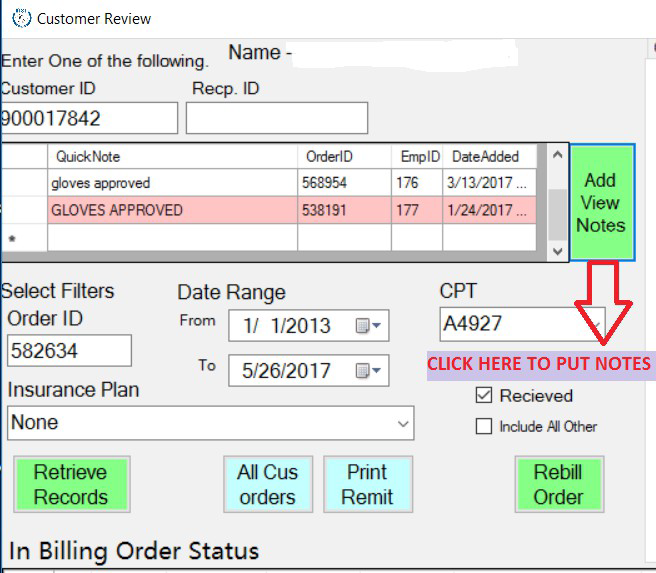
In the CUSTOMER REVIEW WINDOW, click on the ADD VIEW NOTES BUTTON, It should prompt you to go to this page/window: On the QUICK NOTES WINDOW put in the CLAIM STATUS: GLOVES APPROVED |DATE PROCESSED| ORDER ID.
On the note window: Copy paste the CLAIM STATUS, CLAIM ICN and PAID AMOUNT, then click on SAVE. Then you’re good to go.